Your Impact

Every child deserves a chance.
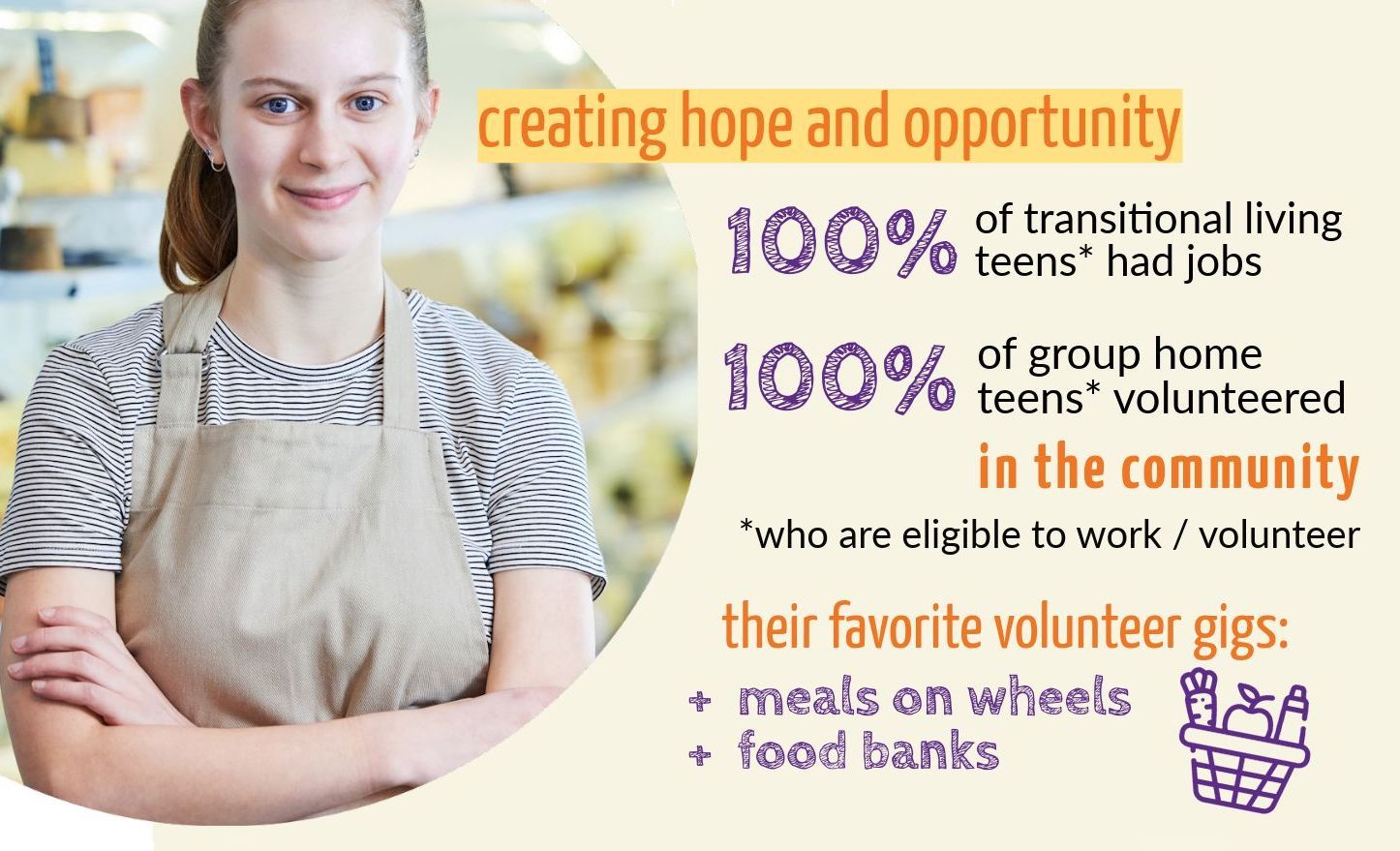
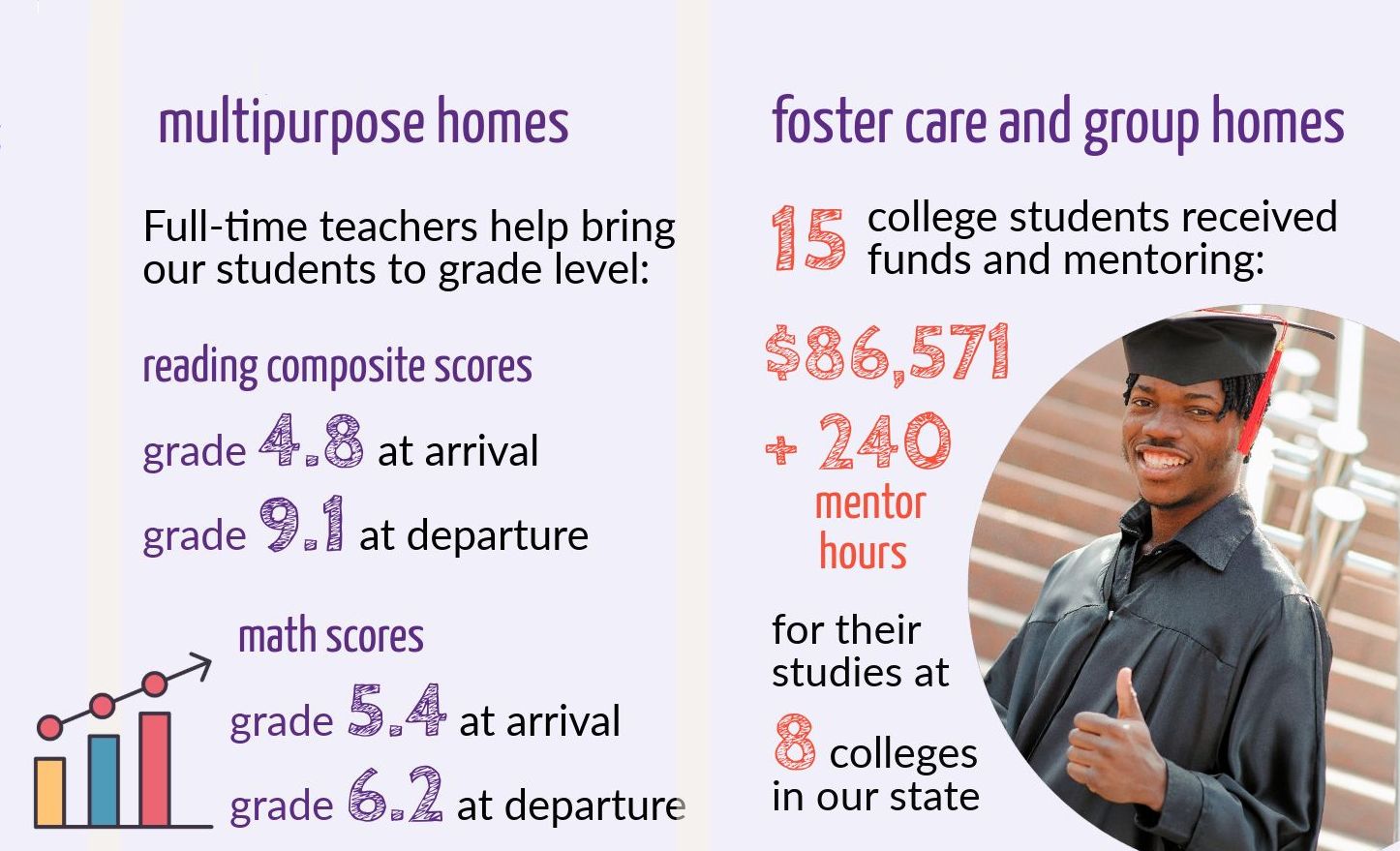
At Methodist Home for Children, we provide safe, stable homes where children can thrive and live to their full, God-given potential. While not always traditional, an MHC home is where child and family are equipped to succeed. We build on strengths, nurturing hopes and goals, and prepare all in our care to shape their own futures.
Your gifts in action – photos and stories delivered monthly to your inbox











